December 23, 2025
2 min read
Key takeaways:
- There was no direct causal relationship between depression and epilepsy.
- Older, smaller studies in the literature review did not confirm the risk.
The risk for a diagnosis of epilepsy is more than two times greater for those with depression, although incidence is low, according to data presented at the American Epilepsy Society annual meeting.
“Our goal was to answer a straightforward question: after a diagnosis of depression, do seizures occur more often?” Ali Rafati, MD, MPH, lead study author and postdoctoral research fellow at Johns Hopkins University School of Medicine, told Healio.

Data were derived from Rafati A, et al. Risk of new-onset epilepsy in people with vs. without depression: A systematic review and meta-analysis. Presented at: American Epilepsy Society annual meeting; Dec. 5-9, 2025; Atlanta.
“The newer, very large datasets consistently show a pattern where depression tends to come first, followed by a higher incidence of epilepsy,” he said.
While prior research has established associations between epilepsy and psychiatric comorbidities, less is known regarding the risk for developing epilepsy in patients with depression, Rafati and colleagues wrote.
As such, they conducted a systematic review and meta-analysis synthesized to quantify the incidence of epilepsy among individuals with and without depression and to identify a clear link between the two conditions.
They utilized the MEDLINE, Embase and PsycINFO databases in search of prospective cohort and case-control studies that examined epilepsy incidence in individuals with and without depression. From an initial set of more than 5,700 records, screening whittled the number of eligible studies down to seven, with an additional study included via hand searching.
The primary outcome measure was the pooled hazard ratio for epilepsy among individuals with a history of depression, while a secondary analysis examined the pooled odds ratio from case-control studies.
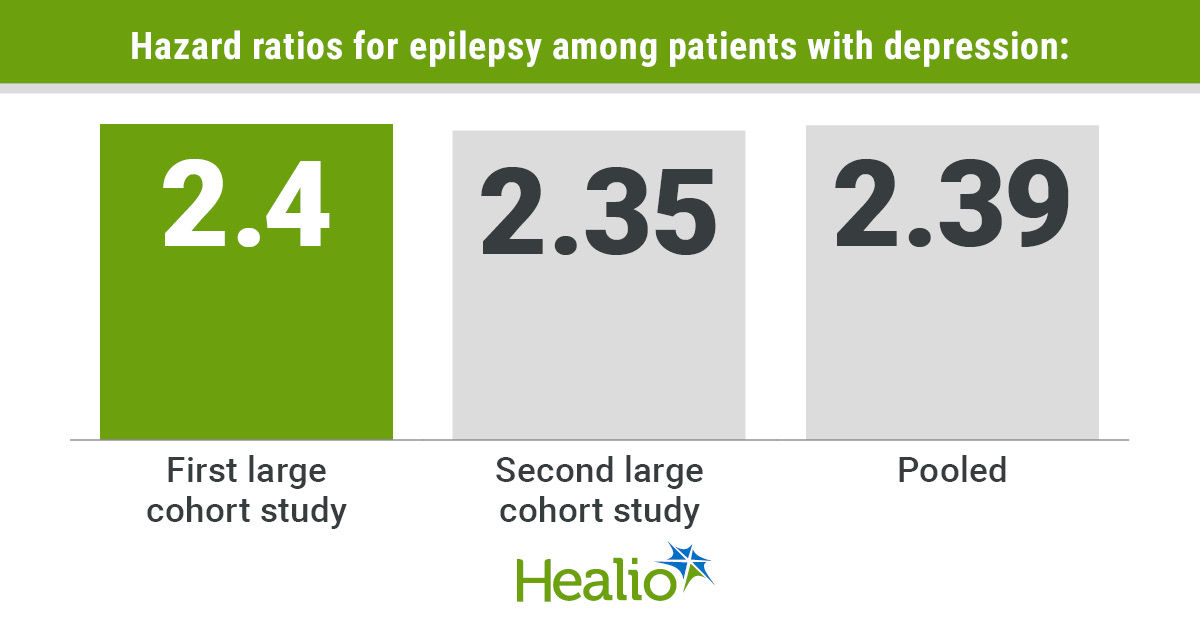
A meta-analysis of two large cohort studies among the eligible research criteria found a pooled HR of 2.39 (95% CI: 2.35 to 2.43). In the first of the two selected, the HR was 2.4 (95% CI: 2.35-2.45) and in the second, 2.35 (95% CI: 2.25-2.44), suggesting a significant increase in epilepsy risk among individuals with prior depression, with low heterogeneity.

Ali Rafati
Conversely, the researchers wrote, secondary analysis of four other smaller case-control studies that examined depression history in individuals with and without incident epilepsy produced a pooled OR of 2.09 (95% CI: 0.92–4.76), with the individual ORs being 1.04, 1.42, 3.18 and 6.33, respectively. These data, they wrote, indicated a high level of heterogeneity despite a lack of statistical significance.
Rafati and colleagues concluded that prospective cohort studies offered the most robust evidence of an association between depression and future risk for epilepsy diagnosis. The retrospective nature of case control studies may be more prone to both recall and selection biases and issues with exposure misclassification, potentially weakening or obscuring the association, they added.
The underlying mechanisms that drive the association need to be fully examined in future studies, along with evaluations that determine whether early identification and management of depression may reduce epilepsy risk, they wrote.
“Clinicians who treat depression should remain aware that neurological symptoms can occasionally overlap,” Rafati told Healio. “If a patient reports episodes that might resemble seizures, such as sudden confusion, unresponsiveness or unusual movements, it is appropriate to explore these further and, if needed, refer the patient for neurological assessment.”
However, Rafati said, this research does not recommend routine seizure screening in all patients with depression, as the majority will never develop epilepsy. Further, he added that clinical decisions should be tailored to the individual, following established care guidelines.
For more information:
Ali Rafati, MD, MPH, can be reached at neurology@healio.com.
#Epilepsy #risk #times #greater #depression






Leave a Reply